This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients’ clinical problems with collective current best evidence-based inputs.
A 35 yr old male patient, bartender by occupation and a chronic alcoholic was presented to casualty.
CHIEF COMPLAINTS:
Shortness of breath since 10 days
Cough since 2 days
HISTORY OF PRESENTING ILLNESS:
The patient was apparently asymptomatic 2 months ago, when he started developing shortness of breath while lying down and on exertion. He also complained of chest pain
1 month ago, they started visiting a local RMP, where he was given an injection? in each visit after which the symptoms used to subside for 10-15days. After this, they visited a doctor and few investigations were done following which he was told to have a heart problem?
Then the patient came to Casualty with complaints of SOB since 10 days
The patient also gave history of cough since 2 days which was mucopurulent.
HISTORY OF PAST ILLNESS:
No h/o HTN
No h/o DM
No h/o allergies
PERSONAL HISTORY:
H/o alcohol consumption since 10 years
H/o passive smoking since 10 years at workplace
Diet : mixed
Bowel and bladder movements : normal
Appetite: normal
FAMILY HISTORY:
No significant family history
EXAMINATION:
General examination:
Patients is conscious, coherent and co operative
Moderately built and nourished
Pallor: absent
Icterus: absent
Clubbing: absent
Cyanosis: absent
Lymphadenopathy: absent
VITALS:
Temperature afebrile
Pulse 140-160 bpm
Respiratory rate : 30 per minute
Bp 130/90
Spo2 98%
GRBS 132 mg%
SYSTEMIC EXAMINATION:
CVS
S1 s2 heard
No murmurs
Respiratory
BAE +
Wheeze + in all areas
ABDOMEN
soft
Non tender
Liver and spleen non palpable
CNS : NAD
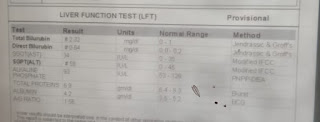
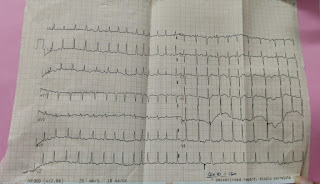
INVESTIGATIONS:
PROVISIONAL DIAGNOSIS:
TREATMENT:
Fluid restriction <1.5L per day
Salt restriction <4gm per day
Inj amiodarone 900mg in 32ml NS
Inj augmention 1.2 gm/IV/BD
tab azithromycin 500mg/PO / OD
Inj hydrocort 100mg IV/BD
Neb duolin, dubocort 8th hrly
Inj lasix 40mg / IV OD
Inj thiomine 200mg in 50ml NS/IV/BD
Inj optineuron 1 amp in 50ml NS IV/OD













Comments
Post a Comment