A 48 YRS OLD MALE PATIENT WAS PRESENTED TO THE OPD WITH COMPLAINTS OF OEDEMA AND SHORTNESS OF BREATH
CHIEF COMPLAINTS:
- cough since 6 months
- shortness of breath since 2 days
- oedema since 2 days
the patient was apparently asymptomatic two and half months ago when he developed fever, burning micturition, pedal oedema which progressed to anasarca, he was diagnosed with AKI and is on maintainance hemodialysis.
2 days ago he had excurbation of shortness of breath especially during night time, oedema and cough because of which he came to the hospital.
HISTORY OF PAST ILLNESS:
h/o diabetes since 4 years
h/o hypertension since 2 years
h/o hypothyroidism since 6 months for which he takes thyronorm 50 mg
FAMILY HISTORY:
no significant family history
PERSONAL HISTORY:
married
h/o consumption of alcohol occasionally
no h/o smoking
diet mixed
normal bowel and bladder movements
GENERAL EXAMINATION:
Patient is conscious, coherent and co-operative
no audible wheeze/stridor
no hoarseness of voice
pallor present
no clubbingg
no cyanosis
bilateral pitting type oedema
CVS:
s1 s2 heard
no murmers
RESPIRATORY:
no dyspnoea
no wheeze
position of tracea- central
ABDOMEN:
liver not palpable
spleen- not palpable
no bowel sounds
CNS:
the patient was conscious coherrent
normal speech
sensory and motor system intact
PROVISIONAL DIANOSIS:
CKD secondary to diabetic nepropaty
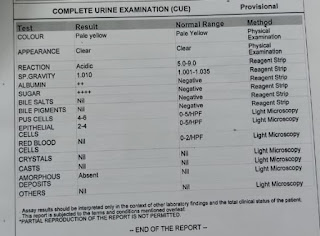
INVESTIATIONS:
TREATMENT:
maintainance haemodialysis
- fluid restriction
- salt restriction
- tab lasix
- tab nicardia
- tab met-xl
- tab tyronorm
- tab uroen
- inj actrapid
- neb budecort-6th hrly ; dubolin - 8th hrly
- tab azitromycin
- tab montek
- syp benadryl













Comments
Post a Comment