A 56 year old male came to the OPD with complaints of abdominal distension from 2 days
CHIEF COMPLAINT :
Swelling of abdomen since 2 days
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 2 and half months back ,then he developed pedal edema -pitting type grade 1 then gradually progressed to grade 2 over 10 days to grade 3 over 15 days
He first developed left lower limb swelling extending upto his ankle and he later gradually developed swelling of his right lower limb and the swelling in both his lower limbs extended upto his thighs
no complaints of fever, cough, burning micturation, loose stools, vomiting
No complaints of dyspnea, hematuria, frothy urine, no complaints of Chest pain, palpitations, orthopnea, PND
HISTORY OF PAST ILLNESS :
H/o pulmonary koch's 22 yrs back ,used ATT for 6 months
HTN since 2 months
PERSONAL HISTORY:
Married
Appetite-decreased
Regular bowel and bladder movements
Occasionally alcoholic
GENERAL EXAMINATION :
Patient is conscious, coherent and cooperative
Moderately built and moderately nourished
Pallor present ,grade 3 clubbing
No Icterus, cyanosis Lymphadenopathy
B/L pitting type upto thighs
VITALS :
Temp: afebrile
PR: 120 bpm
BP: 160/80 mm hg
RR: 24 cpm
Spo2 - 96% at RA
CVS :
S1, S2 heard , No murmurs
RS :
Position of trachea: central
Bilateral decreased air entry +
Expiratory wheeze + in all areas
PER ABDOMEN:
Abdomen distended with no scars, sinuses, engorged veins
No tenderness
Percussion-
Shifting dullness +
Bowel sounds +
CNS:
Patient is Conscious ,oriented to time,place and person
HMF -intact
Motor & sensory system: normal
Reflexes: present
Cranial nerves: intact
No meningeal signs
PROVISIONAL DIAGNOSIS-
NEPHROTIC SYNDROME WITH HTN
INVESTIGATIONS:
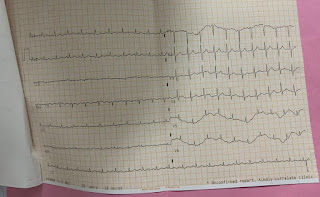
ECG:
Treatment
DAY-1
TREATMENT:
1.FLUID RESTRICTION < 1 LIT/DAY
2.SALT RESTRICTION < 2 GM/DAY
3.TAB LASIX 60MG PO/TID
4.TAB RAMIPRIL 5 MG/PO/BD
5.TAB PAN-D PO/OD
6.MONITOR WT & ABDOMINAL GIRTH DAILY
7. I/O CHARTING
See
DAY-2
TREATMENT :
1.FLUID RESTRICTION < 1 LIT/DAY
2.SALT RESTRICTION < 2 GM/DAY
3.TAB LASIX 60MG PO/TID
4.TAB RAMIPRIL 5 MG/PO/BD
5.TAB PAN-D PO/OD
6.MONITOR WT & ABDOMINAL GIRTH DAILY
7. I/O CHARTING
DAY-3
TREATMENT :
1.FLUID RESTRICTION < 1 LIT/DAY
2.SALT RESTRICTION < 2 GM/DAY
3.TAB LASIX 60MG PO/TID
4.TAB RAMIPRIL 5 MG/PO/BD
5.TAB PAN-D PO/OD
6.MONITOR WT & ABDOMINAL GIRTH DAILY
7. I/O CHARTING
DAY-4
TREATMENT :
1.FLUID RESTRICTION < 1 LIT/DAY
2.SALT RESTRICTION < 2 GM/DAY
3.TAB LASIX 60MG PO/BD
4.TAB RAMIPRIL 5 MG/PO/BD
5.TAB PAN-D PO/OD
6.MONITOR WT & ABDOMINAL GIRTH DAILY
7. I/O CHARTING
DAY-5
TREATMENT :
1.FLUID RESTRICTION < 1 LIT/DAY
2.SALT RESTRICTION < 2 GM/DAY
3.TAB LASIX 60MG PO/BD
4.TAB RAMIPRIL 5 MG/PO/BD
5.TAB PAN-D PO/OD
6.MONITOR WT & ABDOMINAL GIRTH DAILY
7. I/O CHARTING
Day 6-8
1.FLUID RESTRICTION < 1 LIT/DAY
2.SALT RESTRICTION < 2 GM/DAY
3.TAB LASIX 60MG PO/TID
4.TAB PAN-D PO/OD
5.MONITOR WT & ABDOMINAL GIRTH DAILY
6. I/O CHARTING












Comments
Post a Comment