67 year old male patient with CKD
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
Note: This is an ongoing case, the E-LOG will be updated as and when we get the new information.
HISTORY OF PRESENTING ILLNESS:
A 67 year old male patient was presented to the opd with cheif complaints of:
- inablity to urinate and defecate
- shortness of breath
HISTORY OF PRESTENTING ILLNESS:
A 67 year old male patient was presented to the OPD with cheif complaints of Iinablity to urinate and defecate ( defecation only twice a week) , shortness of breath and mild fever.
no h/o cough or pain in abdomen
no h/o vomitings
HISTORY OF PAST ILLNESS:
h/o Diabetes mellitus - since 20 years
h/o hypertension - since 6 months
FAMILY HISTORY :
no h/o any diseases
PERSONAL HISTORY :
diet : non vegetarian
non smoker
non alcoholic
GENERAL EXAMINATION:
conscious and choherrent
moderately built and moderately nourished.
pallor: absent
icterus: absent
cyanosis : absent
clubbing: absent
edema : absent
lymphadenopathy: absent
VITALS:
BP: 120/70 mmHg
PR: 80 bpm
Systemic Examination:
CVS:
inspection:
- chest wall is bilaterally symmetrical
- no visible pulsations,engorged veins, scars and sinuses
- jvp: normal
- apex beat: felt in 5th intercoastal space in mid clavicular line
auscultation:
- s1 s2 heard
- no murmurs
RESPIRATORY:
- central position of trachea
- bilateral air entry: positive
- normal vesicular breath sounds are heard
- no added sounds are heard
PER ABDOMEN:
- abdomen distended, soft and non tender.
- bowel sounds heard
- no palpable mass or free fluid
CNS:
- no focal neurological deficits
INVESTIGATIONS:
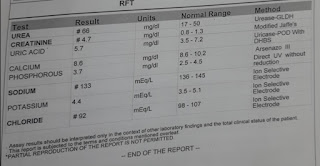
RENAL FUNCTION TEST:
COMPLETE BLOOD PICTURE:
HCV TEST:
BLOOD GROUPING:
HIV TEST :
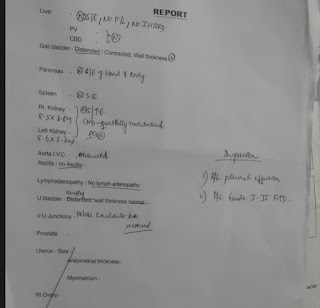
ULTRA SOUND REPORT :
DIAGNOSIS:
Chronic Kidney Disease on MHD
PLAN OF CARE:
maintenance haemodialysis
Blood transfusion ( occured on 10/7/21 )
TREATMENT:
on 11/7/12
- fluid restriction < 2 L/day
- salt res triction < 2 gms/ day
- Tab. Lasix 40 mg PO BD
- Tab. shelcal 500mg PO OD
- tab nodosis 550 mg PO OD
- Tab orolex XT PO OD
- Tab Nicardia 10 mg PO BD
- I/O charting
- GRBS charting 6th hourly
- BP charting 8th hourly
- Inj. HAI / s/c /
on 12/7/21
- fluid restriction < 2 L/day
- salt res triction < 2 gms/ day
- Tab. Lasix 40 mg PO BD
- Tab. shelcal 500mg PO OD
- tab nodosis 550 mg PO OD
- Tab orolex XT PO OD
- Tab Nicardia 10 mg PO BD
- I/O charting
- GRBS charting 6th hourly
- BP charting 8th hourly
- Inj. HAI / s/c /
- inj ceftriaxone 1mg IV BD
- inj pan 40mg IV OD
on 13/7/21
- fluid restriction < 2 L/day
- salt res triction < 2 gms/ day
- Tab. Lasix 40 mg PO BD
- Tab. shelcal 500mg PO OD
- tab nodosis 550 mg PO OD
- Tab orolex XT PO OD
- Tab Nicardia 10 mg PO BD
- I/O charting
- GRBS charting 6th hourly
- BP charting 8th hourly
- Inj. HAI / s/c /
- inj ceftriaxone 1mg IV BD
- inj pan 40mg IV OD
on 14/7/21
- fluid restriction < 2 L/day
- salt res triction < 2 gms/ day
- Tab. Lasix 40 mg PO BD
- Tab. shelcal 500mg PO OD
- tab nodosis 550 mg PO OD
- Tab orolex XT PO OD
- Tab Nicardia 10 mg PO BD
- I/O charting
- GRBS charting 6th hourly
- BP charting 8th hourly
- Inj. HAI / s/c /
- inj ceftriaxone 1mg IV BD
- inj pan 40mg IV OD
- inj erythropoietin 1000 units weekly twice
HEMODIALYSIS CHART





Comments
Post a Comment